Pain in the lower part of the abdomen is coined as pelvic pain. It can be gynaecological or non gynaecological (Table 1). It can be further classified as acute (sudden onset) or chronic (more than six months).
Table of Contents
Gynaecological causes of pelvic pain are:
Ovulatory pain
Menstrual pain/Dysmenorrhea
During period, there is a chemical released in our body, called prostaglandin, which causes our womb to go into spasm. This spasmodic pain is referred as menstrual pain.
Endometriosis
This is a common condition affecting menstruating women. The exact mechanism causing endometriosis is still unknown, but common theories are, backflow of blood through the fallopian tube during menstruation and a lowered body immune system.When the cells lining the uterus are found outside the womb, it is called endometriosis. Due to the natural hormonal influence, the cells outside the womb, can grow and bleed during menses. Over time, these blood and tissues will build up, causing pain and swelling.Treatment for endometriosis is painkillers, hormonal pills or surgery
Pelvic inflammatory disease
This is infection in the fallopian tubes and sometimes, ovaries too. Commonly occurs in sexually active women, especially if there are more than one sexual partner.Treatment is with antibiotics for both partners and barrier methods of contraception should be discussed.
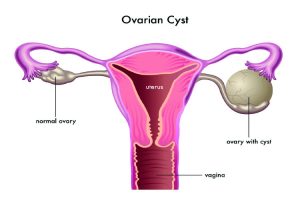
Non cancerous growths of the genital tract
Fibroid is a very common benign(non cancerous) growth in our womb. Large fibroid can cause pain. Ovarian cysts are also common. When the size is big, it can burst or twist on its pedicle, causing pain. Treatment of fibroid and ovarian cyst depends on the size and symptoms that it is causing.
Cancerous growths in genital tract
Generally, pain is not a feature of pelvic cancer. But, when the mass is big in advanced cancer, it can cause pain in the pelvis or abdomen
Adhesions
Adhesion means tissues inside our abdomen are adhered together and this can cause pain. It can occur after any previous operation, infection or inflammation within the abdominal cavity.
Pelvic pain syndrome
This normally causes chronic pelvic pain.When the pelvic pain is unexplained, congestion of the pelvic veins (blood vessel) is thought to be the root of the problem.This is described as fullness of the pelvic blood vessels and only happens to women who are still menstruating.The pain is normally described as a dull ache in the lower right side of the abdomen, and sometimes be severe and can move from side to side.The pain tends to respond to postural change, lying flat relieves the pain whilst movement aggravates it.Treatment can be by reassurance, painkillers or psychotherapy. In the majority of women, pain will resolve spontaneously when investigations showed no abnormalities.
Uterovaginal prolapse
This is a condition where the womb is dropping out, down below, because of weakened pelvic floor muscles.
Bowel
Colon infection, inflammation, obstruction, cancer can all cause pelvic pain.
Urinary tract
Urine infection, stones, cancer and urine retention (cannot pass urine) can cause pelvic pain too
Muscles & bone related
Arthritis, spinal disc prolapsed, muscular strain can contribute to pelvic pain as well.
Pelvic floor dysfunction
This can be due to tight pelvic muscles or loose pelvic muscle. Sometimes, pelvic floor dysfunction can also result in impairment of the hip joint, lower back and coccyx. Pelvic floor dysfunction can present as urinary incontinence, fecal incontinence, pelvic organ prolapsed, sexual dysfunction, pelvic pain. The commonest conditions experienced in pelvic floor dysfunction are urinary incontinence, anal incontinence and pelvic organ prolapsed. For all intent and purposes, pelvic floor dysfunction is normally associated with loose muscles rather than tight muscle. As such, the latter will not be mentioned in this article as there is no definitive diagnosis or treatment for it, except stretching of the vaginal wall or psychotherapy.
Causes of weakened pelvic floor:
Childbirth
Prolonged labour and big baby can weakened the pelvic floor muscles because of prolonged stretching of the muscles.
Chronic raised intra-abdominal pressure
Chronic heavy weight lifting, chronic cough, chronic constipation, prolonged standing can exert constant pressure on the pelvic floor causing its weakening.Obesity has also been associated with increased abdominal pressure on the pelvic floor.
Ageing
As we aged, our muscle will weaken and loses its elasticity. This can lead to a weakening and loss of strength of the pelvic floor. Menopause can aggravate the loss of the elasticity due to lack of the oestrogen hormone.
Symptoms of pelvic floor prolapsed:
‘A lump down below’ is a common complaint of patients suffering from pelvic floor prolapsed.
The lump will disappear upon lying down and is more pronounced at the end of the day.
Backache
This is due to stretching of the muscles and ligaments of the pelvic floor when the womb hangs out from the vagina.
Urinary symptoms
Difficulty in passing urine, increase frequency of passing urine, urinary incontinence when cough/sneezes or when couldn’t get to a toilet in time, are common symptoms in womb prolapse. This can be due to urine retention in a prolapsed bladder or an unstable bladder muscle.
Difficulty in passing faeces
It may be difficult to empty the bowel when the bowel prolapsed into the vagina. Patient often has to push the bowel back from the vagina before they can open their bowel.
Vaginal bleeding
When the uterus is out of the vagina, it can rub against the underpants causing bleeding or pain. Over time, ulcer can develop in this exposed part and infection may happen.
Treatment of prolapse:
Prevention.
- During childbirth, avoid prolonged labour. Repair any tissue tear accurately in layers during childbirth. Encourage pelvic floor exercise post childbirth to re-strengthen the muscle.
- Avoid heavy lifting, obesity, prolonged standing.
- Treat chronic cough adequately
- Avoid chronic constipation
Definitive treatment
Ring pessary 
This is a flexible, non irritating PVC ring that is inserted into the vagina to support the uterus and vagina, up the pelvis. It does not cure the prolapse. It is commonly used in elderly patient who are not fit for surgery, or in women of childbearing age, who still desires future pregnancies. The ring has to be changed every 6 months for hygiene purposes. It can sometimes cause vaginal infection or ulceration, leading to bleeding in prolonged use. But these symptoms can be treated easily.
Surgery.
Operation will be considered in young, fit women who are still sexually active, as the use of the ring pessary will hinder their sexual activities. Surgery can also be contemplated in women where ring pessary has failed. Prior to surgery, obesity, constipation have to be treated to reduce the risk of the vagina prolapsing out in the future. Heavy lifting post operation is also discouraged for the same reason.


















