The science involved in the treatment of infertility has rapidly advanced in the past few years . This advancement is clearly seen in the field of In-Vitro Fertilisation or IVF.
Current technology enables us to look into the genetics of human reproduction. Genetic testing also provides answers to infertility; and in some cases, solutions.
Preimplantation Genetic Screening (PGS)
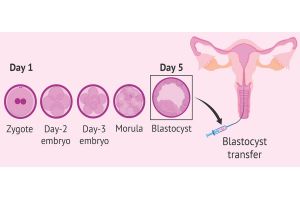
IVF involves creating embryos in an IVF laboratory and placing them into the womb.
Traditionally an embryo is graded based on its morphology (external appearance under a microscope). The embryo/embryos with the best gradings is/are transferred back into the womb.
A morphologically-normal embryo with the best grading does not necessarily indicate that the embryo is genetically normal (euploid embryo).
A genetically-normal embryo will lead to a successful pregnancy, assuming there are no other factors contributing to a failed embryo implantation or pregnancy. Preimplantation genetic diagnosis (PGS) looks at the genetic normality of the embryo prior to an embryo transfer procedure. Embryos are typically grown up to 3 to 6 days before the biopsy is performed.
Biopsy of the embryos are done when the embryo is either 3 days old or when they have reached Day 5 or 6, known as a blastocyst.
Biopsy of the blastocyst is usually preferred because more cells are obtained from the embryo thus increasing the chances of the PGS to be performed successfully.
To be able to perform the biopsy, a small opening is made on the outer layer of the embryo, using either mechanical, chemical or laser technology. The biopsied cells (usually in the range of 5-10 cells if done on a blastocyst or 1-2 cells if done on Day 3 embryo) are then amplified to make a large number of copies of the genes to be studied. To be able to perform PGS on the embryo/s, the couple need to go through an IVF procedure to create an embryo in the fertility laboratory and the embryo/s is/are typically frozen, pending the PGS results.
A PGS-normal embryo/s is/are then transferred into the womb. This process is know as frozen embryo transfer (FET). FET is done either in a natural cycle or in a hormone replacement cycle.
Genetics of Male Infertility
About 15% of couples have infertility. At least 40-50% of them have male factor related infertility.
Male infertility ranges from very low sperm quantity (severe oligospermia) to no sperms cells (azoospermia), apart from sperm quality issues.
Genetics testing for a man is important especially if he suffers from azoospermia and to a lesser extend, severe oligospermia. This genetic testing is done from the blood sample of men. Both women and men have 23 pairs of chromosomes, out of which one pair will determines the sex of the fetus (sex chromosomes). There are two sex chromosomes, X and Y.
A man carries the XY chromosome while a woman carries the XX chromosome. Up to 10-15% of men with azoospermia and about 5% of men with severe oligospermia have a gene deletion on chromosome Y. This is known as microdeletion-Y. There are generally 3 types of microdeletion-Y, namely AZF-a, AZF-b and AZF-c.
In an individual with microdeletion-Y with AZF-a, there is about 50% chance of retrieving sperm directly from testicle of the man. However, in complete AZF-b and AZF-a deletions, it’s nearly impossible to retrieve sperm surgically from testicles.
Some men with azoospermia may have a condition called Klinefelter Syndrome. This happens in about 3% of men with azoospermia. In Klinefelter syndrome, the man has an extra X sex chromosome thus the chromosome are often detected as 47-XXY. Men with this syndrome have a certain typical physical attributes, however some men with this syndrome may not exhibit the typical features.
Azoospermia can also be due to absence of vas deference (tube that transport sperm out of testicles). This condition is called Cystic Fibrosis which is due to mutation in the cystic fibrosis gene (CFTR). This condition is uncommon in Asian population.
Genetic tests for recurrent
Couples with recurrent miscarriages or couples who underwent an IVF with recurrent implantation failure may need to test their own genetics (chromosome test).
In some cases, couples do carry an abnormality in their chromosomal arrangement, known as balanced translocation. A balanced translocation does not cause problem in the affected individual. However, once the translocation has been passed down to their offspring, it can become ‘unbalanced’. An unbalanced translocation can lead to a pregnancy loss and implantation failure in an IVF.
Genes that are linked to development of immunotolerence to the fetus, inflammation and genes that alter maternal metabolism and blood coagulation are also being studied. In conclusion, couples who are dealing with infertility, recurrent miscarriage and repeated IVF failures should discuss with a fertility doctor about appropriateness of genetic testing for them.